Being diagnosed with type 2 diabetes can feel overwhelming, confusing, and even frightening. You may be wondering what led to it, whether medication is your only option, and if there’s a way to turn things around.
The good news is, you have more control than you might think. Moreover, taking action now can lead to lasting improvements in your health.
In this article, we’ll explain what type 2 diabetes is, what causes it, and how a well-formulated ketogenic diet can help you manage your blood sugar and, in many cases, even reverse the condition.
What Is Type 2 Diabetes?
Type 2 diabetes is a condition that usually develops because the body is no longer using insulin effectively due to insulin resistance. Insulin is the hormone that helps move glucose (sugar) from the bloodstream into your cells to be used for energy. When a person has insulin resistance, their cells are less responsive to insulin’s action. As insulin resistance sets in, the pancreas works harder to produce more insulin in an attempt to keep blood sugar levels stable. Over time, however, it may not be able to keep up with the demand, leading to rising blood glucose levels.
When glucose builds up in the bloodstream instead of entering the cells, the result is high blood sugar, also known as hyperglycemia. If not properly managed, this condition can progressively cause serious complications, such as damage to the blood vessels and nerves in the eyes, kidneys, and heart, and may ultimately lead to amputations. Indeed, the American Diabetes Association reports that in the US, every four minutes a limb amputation takes place due to diabetes. Diabetes is also the leading cause of end-stage kidney disease requiring dialysis. Moreover, people with diabetes are at a significantly higher risk of developing cardiovascular disease and experiencing heart attacks, heart failure, and strokes that lead to disability or death. Diabetes-related problems often develop slowly and may not cause noticeable symptoms early on. In addition to problems caused by hyperglycemia, elevated insulin levels, known as hyperinsulinemia, can also increase risk of cardiovascular disease, cancer, and obesity.
In many cases, type 2 diabetes is preceded by prediabetes, a stage where blood sugar (and insulin) levels are elevated but not yet high enough to be diagnosed as diabetes. Because prediabetes typically has no clear symptoms, many people are unaware they have it, despite its strong link to an increased risk of developing type 2 diabetes.
Why Did This Happen?
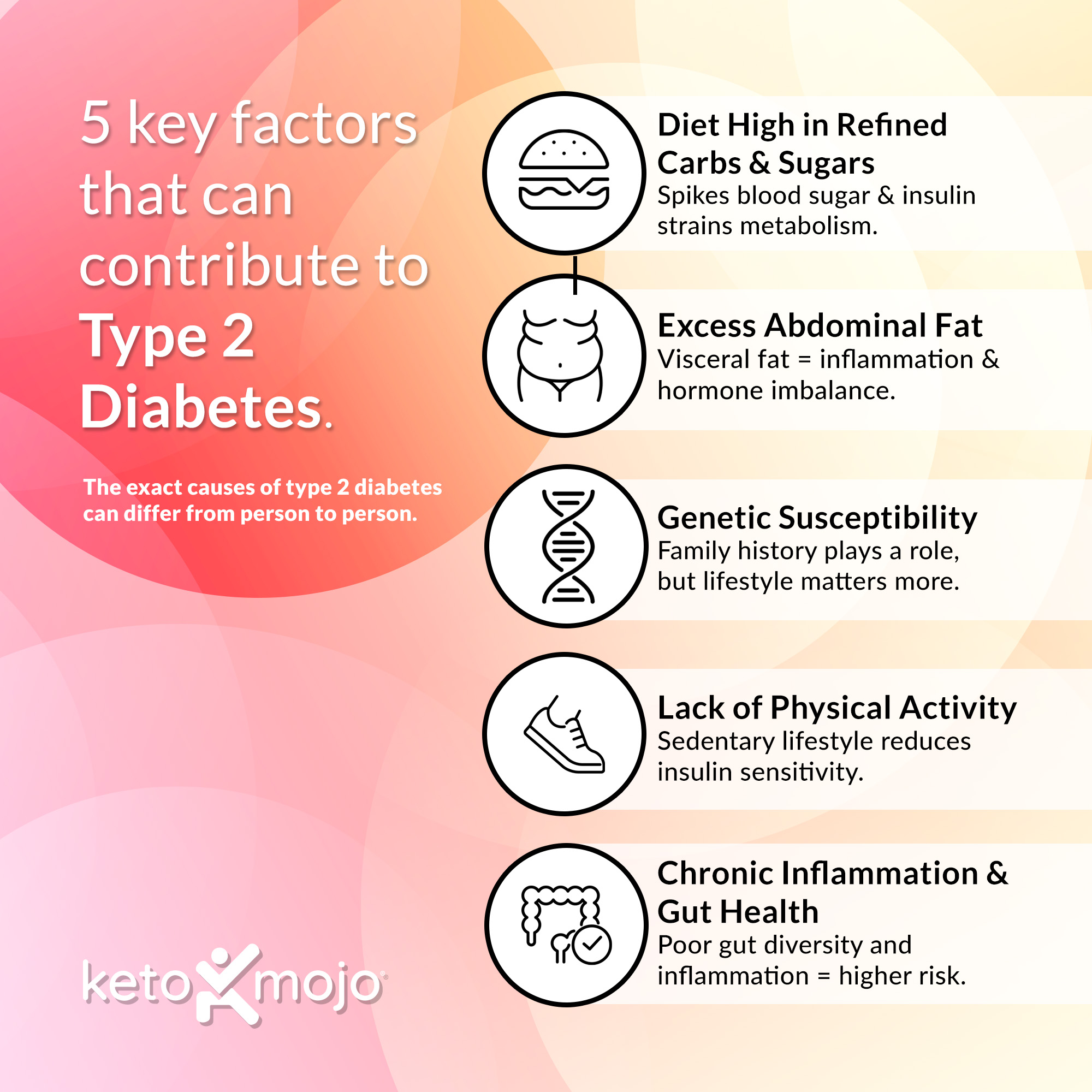
While the exact causes of type 2 diabetes can differ from person to person, several key factors often contribute:
- Diet high in refined carbohydrates and sugars: Consuming processed carbs, sugary treats, and sweet beverages can cause repeated spikes in blood glucose and insulin levels. Over time, this may place stress on the body’s metabolic system and contributes to poor blood glucose control and other health problems.
- Excess abdominal fat: Fat stored deep in the abdominal area (visceral fat) is particularly metabolically active and is linked to increased inflammation and hormonal imbalances that impair glucose regulation.
- Genetic susceptibility: While type 2 diabetes can run in families, genetic risk is only one piece of the puzzle. Even with a strong family history of diabetes, lifestyle choices — such as diet, activity, and stress management — can greatly influence whether or not someone develops the condition.
- Lack of physical activity: Regular movement can help improve how the body handles glucose and supports overall metabolic health. A sedentary lifestyle, on the other hand, reduces insulin sensitivity and can increase the risk of developing type 2 diabetes.
- Chronic inflammation and gut health imbalance: Emerging research points to a connection between systemic inflammation, poor gut microbiota diversity, and metabolic diseases, including type 2 diabetes.
The silver lining? Lifestyle changes – especially dietary ones – can make a huge impact on the course of this disease.
Can It Be Reversed?
While type 2 diabetes is officially considered a chronic, progressive condition, remission is entirely possible, especially when caught early. The term “diabetes remission” is defined by international consensus as maintaining an HbA1c below 6.5% for at least three months without the use of any diabetes-specific medications.
A ketogenic diet – a very low-carbohydrate, high-fat, moderate-protein way of eating – may help reverse type 2 diabetes by targeting its root causes. By dramatically reducing carbohydrates, this way of eating shifts the body into nutritional ketosis, a state where fat replaces glucose as the body’s primary fuel source. This can lower insulin levels, improve insulin sensitivity, reduce blood sugar, and promote fat loss, especially around the abdominal area.
Several clinics now offer programs focused on type 2 diabetes reversal using a ketogenic approach. One example is Virta Health, which helps individuals achieve and maintain nutritional ketosis with ongoing support from remote care clinicians and health coaches. The company has also published some of the most well-known long-term research using this approach in people with type 2 diabetes. In their first published paper led by Dr. Sarah Hallberg, researchers reported one-year outcomes from an ongoing continuous remote care intervention in adults with type 2 diabetes. Participants who followed a ketogenic approach experienced significant improvements in blood sugar, a 55% reduction in insulin resistance, and were able to stop or reduce insulin in 94% of cases – all without reported adverse effects. In a two-year update published by Dr. Shaminie Athinarayanan, 55% of participants who stayed in the program achieved diabetes reversal, which is defined by Virta as reaching an HbA1c below 6.5% without the use of diabetes-specific medications other than metformin. On average, participants lost 26 pounds and were able to significantly reduce or eliminate medications, including insulin.
In an extension of the same study, Dr. Amy McKenzie and colleagues published data from participants who chose to continue the program beyond two years. At the five-year mark, 20% of those individuals achieved diabetes remission, meaning they achieved an HbA1c below 6.5% for at least three months without any diabetes medications. Participants also maintained an average 6% weight loss, reduced their triglycerides, and improved markers of inflammation.
Dr. David Unwin, a general practitioner in England, has successfully implemented a very-low-carbohydrate diet in his practice since 2013, helping 51% of participating patients with type 2 diabetes achieve remission. His approach led to significant improvements in weight, HbA1c, lipid levels, and blood pressure, along with substantial cost savings on diabetes medications.
These results show that a well-planned ketogenic diet, supported by clinical care, can lower blood glucose in people with type 2 diabetes, improve their overall metabolic health, and even help reverse the condition.
What Can I Do Now? (Your 5-Step Action Plan)
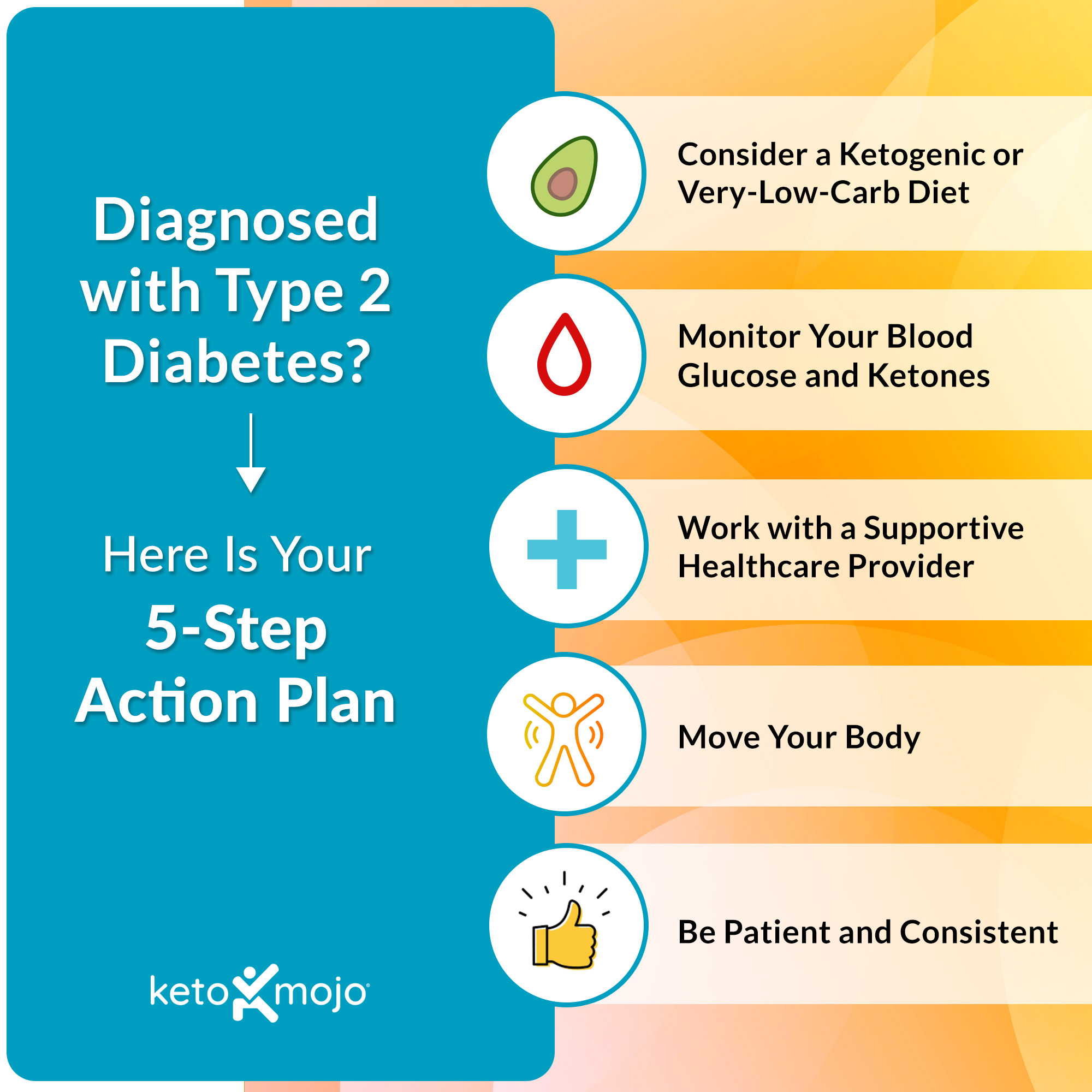
If you’re interested in making lifestyle changes to manage your type 2 diabetes, here are some steps to consider for getting started.
1. Consider a Ketogenic or Very-Low-Carb Diet*
Before beginning a ketogenic diet, learn more about what it involves by reading our article What is the Ketogenic Diet?
If you prefer to start more slowly you can start gradually by cutting out sugar and processed foods, and then lower your intake to less than 30 grams of net carbs (or 50 grams of total carbs) per day.
Focus on non-starchy vegetables (leafy greens, broccoli, cauliflower). healthy fats (olive oil, avocados, nuts), high-quality proteins (eggs, poultry, fish, meat, cheese, plain full-fat yogurt), and minimally processed foods
Avoid starches (bread, pasta, rice, potatoes), sugar, sweets, and sweet drinks, and most processed foods and snacks
For a comprehensive food list, see What Do I Eat on the Keto Diet? What Foods Can I Have?
IMPORTANT: If you take diabetes medication or medication to lower your blood pressure, be sure to speak with your doctor prior to making any changes to your diet.
2. Monitor Your Blood Glucose and Ketones
Testing your blood glucose and ketones helps you understand how food, physical activity, and stress impact your metabolic health. To track your progress and stay safe:
-
- Learn about your ideal glucose levels in What Should Your Glucose Levels Be?
- Confirm you’re maintaining ketosis by finding your target range in What Should Your Ketone Levels Be?
- Unsure about when to test? See When to Test Your Ketones and Glucose.
3. Work with a Supportive Healthcare Provider
Regardless of whether you are currently taking medication for diabetes, it’s important to let your doctor know that you plan to begin pursuing a ketogenic or low-carb approach. Show them this article and the supporting studies linked to at the end.
Diabetes medication doses — especially insulin or sulfonylureas — may need to be reduced immediately to avoid hypoglycemia (dangerously low blood sugar). Similarly, antihypertensive medications may need to be reduced in order to avoid dangerously lower blood pressure.
If your doctor is not supportive of reducing carbohydrates, consider enrolling in the Virta Health program or working with a clinician listed in the Society of Metabolic Health Practitioners directory.
4. Move Your Body
Regular physical activity is a vital component of managing diabetes. It lowers blood sugar, protects insulin-producing cells, and reduces inflammation, which supports better glucose control and overall metabolic health. Even walking for 15 minutes after a meal can be helpful. In addition, research suggests that taking short breaks to walk up and down stairs – even for just 3 minutes – after eating can help lower blood sugar and insulin levels, with longer bouts of 10 minutes or more offering added benefits for improving insulin sensitivity.
5. Be Patient and Consistent
Sustainable lifestyle change takes time, so go easy on yourself and celebrate small wins. Keep in mind that even modest improvements in blood glucose and weight can lower risk of complications and improve your quality of life.
Take Home Message
A type 2 diabetes diagnosis can feel overwhelming, but it doesn’t have to define your future. With the right support, knowledge, and sustainable lifestyle changes – including a ketogenic or low-carb diet – many people are improving their health and even reversing the condition.
By taking the first step, it’s entirely possible to gain control of your blood sugar and work toward lasting remission.



